Stressful night shift:
Arrive on my night shift in a good mood. Final night of 3 and not short-staffed. Have the same patients as yesterday who are stable. Get bedside handover, day nurse reports a long difficult shift, so feel grateful that the night is expected to be more quiet. People often say emergencies are more likely to happen in the night on our ward but felt optimistic.
Go to the patients to see how they are and make a baseline clinical assessment. One female patient was comfortable in bed but just frustrated as was expecting to have an ultrasound today and go home tomorrow. Our interactions involved her wanting updates on whether her scan would be tonight. Gave her medications and no issues at the time.
As the night went on, this patient had an episode of diarrohea but no abdominal pain and seemed to pass quickly. I escalated to NIC and put oxygen on the patient as she felt exhausted from her toilet trip. Made her comfortable in bed and hoped she would get a good nights sleep
Went for my evening break at 00:00 and come back to find my patient in distress. Her observations all looked okay on the monitor but she was breathing fast and said she couldn’t get comfortable. I did a full clinical assessment including measuring her blood sugar and ECG to ensure we weren’t missing anything- everything looked okay.
Our patients have ECG monitors attached to them that continuously measure their heart rate and rhythm. The machines are very sensitive so if a patient moves or a lead falls off it can trigger a false alarm. My patient’s monitor kept going off so I flagged to the doctor but nothing abnormal came up and she was frequently repositioning. I gave her some nebulisers to help with her breathing and then attended to another patient in the bay who was NEWS scoring. It was difficult trying to manage my time to support both patients who appeared unwell.
My female patient still felt unwell but now had pain in her neck. I went to check the site and felt that her skin was cold and clammy. I escalated to our critical care outreach team and called the night SHO to come review the patient immediately. Whilst the doctor was present, tried to re-check the patient’s blood pressure however unable to retrieve a reading. Her temperature had dropped to 34.2. The weirdest but most reassuring part was she was fully alert and verbalising her needs, even making jokes.
I put 15L oxygen on her and went to retrieve cardiac drugs that were required. I then tried to re-check her BP- 84/48. Her saturation and heart rate weren’t retrievable as her hands were too cold for the pulse oximeter to detect the readings.
Then everything happened quite fast. The critical care outreach and anaesthetist came and tried to establish IV access or blood gas but unsuccessful initially. I then put out a cardiac arrest call and a whole swarm of night doctors and nurses came to attend.
The working diagnosis became that she is having a cardiac tamponade and needed to be taken to theatre asap to drain the blood encasing her heart. With all her different lines attached, we wheeled the bed down 3 floors below to rush her to surgery.
The patient was still alert so I let her know I was with her so she wasn’t frightened and had a familiar face. Once the surgery began I was dismissed and returned to the ward to resume care for my other 5 patients.
I then had a real panic about the night’s events and felt very emotional. I didn’t know what to do with myself as everything felt very surreal. It was a very weird feeling to recognise that a lot of what enabled me to escalate my patient’s deterioration early was reliant on a gut feeling/bad intuition. The clinical observations all reported everything was normal. It was also very unexpected- this patient was meant to be going home and had been fit and well otherwise
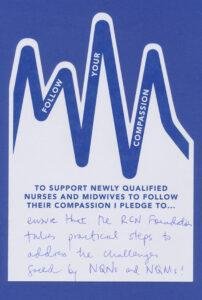
What I truly valued in this experience was the compassion of my colleagues. The nurse in charge reassured me that I had done everything correct and caught the emergency early. I still struggled to believe her though and felt guilty, racking my brains to figure out what more I could have done. She gave me a hug at the end of the shift and I think this helped more than any verbal reassurance.
The night doctor on the ward also came to speak to me. He gave me such kind words of affirmation and offered to give me a letter of appraisal for the work I had done. He brought me a flower to cheer me up. I was incredibly grateful that he took my escalation calls seriously and came to the patient with a matter of urgency. He kept very calm and collected throughout the emergency and thus I felt competent in my care.
It has reiterated for me the reason I chose to work on this ward- it is an environment where I feel completely supported by my colleagues and can trust them in any emergency.
When I get home from work, time seemed to pass very quickly as if the adrenaline rush was still going. To unwind I made breakfast, decompressed the day with my flatmate and then went to sleep.
Flower pic:
Entry two:
It has been nice moving to a new flat and living closer to the hospital as only takes me 10 mins by train to get in. Means I get more precious me time in the morning. Arrive at work and put my stuff in my locker and prepare a sugary drink to keep me going throughout the shift. I have started to bring a book to work, normally something a bit trashy, as it helps me to disconnect from the ward tasks/alarms on my breaks. You can always hear the heart monitors that patient’s wear alarming- this sound is quite triggering as it can either mean a real emergency or they have knocked off a lead/are moving around the ward (AUDIO CLIP attached below). At lunchtime when I have more time I go to the well-being centre to have a physical distance from the ward and reset. It is my favourite space because it is an old building that’s features don’t resemble a hospital. Feels like I am sitting in a library and has nice reclining seats.
Something that is broken in my workplace is that the break room is too small- you can’t fully relax in a tiny box room where people come in and out to use the microwave. Something that is brilliant is the fountain in the square- having an outdoor space on site makes the work environment feel more homely. I remember as a child coming to the fountain with my mum who worked at the hospital and how excited I was to come into work with her.
There are lots of rules in my place of work as patients follow a strict surgical pathway and have clinical milestones to meet in order to be medically fit for discharge. But I also like that nurses are empowered to make clinical judgements on a patient’s progress and manage their care on the ward. For example, we have a checklist for each day post-op to monitor patient’s progress in eating, micturition, mobility, lines, heart rate and rhythm and breathing.
The reason I work here is because it is a very positive working environment. Everyone mucks in to make sure the patient’s feel cared for and it feels like a shared responsibility. In an emergency I know any person I picked to help would come immediately and know what to do. It gives you a true sense of community rather than fostering a destructive blame culture.
One of the emergency bells goes so I run to our central monitor to see which patient is in need of urgent care. The patient is on the adjacent ward- I pick up a glucose machine on the way to the bed. Arrive and patient is had fainted but was now awake and talking- great sense of relief. Lots of people attending slowly leave. As I am leaving the ward, another emergency bell. This time it was a false alarm- the patient was trying to press the call bell for a cup of tea.
An example of flourishing leadership is having your presence felt on the ward and it being a positive influence. I think seeing your leader in the clinical environment but also seeing them perform clinical tasks fosters your trust in their knowledge and care advice. Knowing that you can come to them with any question or problem and will be received kindly and empowered to find the solution. Even when they are very busy, providing you with time and care.
The view from my main place of work looks onto a banking building. They have a bar with flat screen tv’s and often a spread of nice snacks. Feels weird to look onto their lives and know they are probably making a lot of money but wondering if they are satisfied. I also wonder whether they think the exact same looking back at us or maybe their windows have been purposely blacked out
Time felt slow when I was in control of my workload and fast when increasing ward demands make me feel pressured.
Something I wish people asked me rather than “are you okay”, is something more personal about what interests me or what I enjoy doing.
The most important objects here are working computers and machines as our whole day revolves around them, and having them functioning and accessible means I can fulfil my tasks without delay, de-stress, and spend more time with the patients. I would love to be able to sit down and really chat to my patients rather than have all our interactions be clinically motivated.
Ironically, the objects that get in the way of my work are normally the same machines if they are faulty or there is not enough of them. It means a clinical task can take double the time, and then you can easily receive more backlash from the medical teams for not getting things done efficiently.
Belonging means to me that all team members feel responsible for each other’s happiness. i.e. I feel responsible for not only my well-being but wanting my colleagues to have a good, stress-free shift.
At the end of a shift I listen to upbeat music, have something sweet to eat when I get home and then journal and Netflix to withdraw from the day.
Compassion in the workplace today: Nurse educator coming to do on ward training with me. Giving me positive feedback, letting me know that people are looking out for me and giving me realistic timeframes to get competencies done.